Chinese Neurosurgical Journal Study Reveals High Paralysis Risk in corticospinal tract-Infiltrating Gliomas
Gliomas invading the brain’s motor pathway significantly increase long-term paralysis risk, highlighting urgent need for cautious surgical strategies
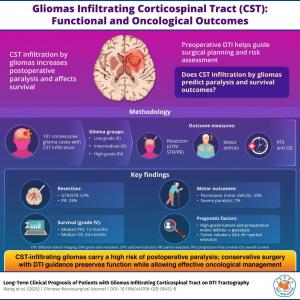
BEIJING, BEIJING, CHINA, December 11, 2025 /EINPresswire.com/ -- Researchers at Beijing Tiantan Hospital analyzed 101 glioma cases involving the brain’s motor pathway and found that one-third of patients developed permanent paralysis after surgery. High tumor grade, pre-operative motor deficits, and larger tumor volume were key predictors. The work underscores the need for precise imaging and careful surgical planning to maximize survival while safeguarding motor function.Gliomas that invade the brain’s motor pathways pose some of the most difficult challenges in neurosurgery, often forcing surgeons to choose between maximizing tumor removal and preserving a patient’s ability to move. A new long-term study sheds critical light on how infiltration of the corticospinal tract (CST)—the brain’s key motor highway—impacts patient function, surgical planning, and survival.
The study, conducted by researchers from China, led by Tao Yu from Beijing Tiantan Hospital, along with Xijie Wang and Songlin Yu from the same institute, and conducted in collaboration with Zhentao Zuo of Chinese Academy of Sciences, was published in Volume 11 of the Chinese Neurosurgical Journal on 24 October, 2025. It provides a comprehensive analysis of 101 patients whose gliomas had infiltrated the CST based on preoperative diffusion tensor imaging (DTI) tractography.
The research team followed patients for a median of more than four years, providing an unusually long and detailed look at both functional and oncological outcomes. They found that CST infiltration is strongly associated with long-term motor deficits: nearly one-third of patients experienced permanent paralysis after surgery, despite careful intraoperative monitoring using direct electrical stimulation. “Even with advanced mapping tools, CST infiltration fundamentally limits how much tumor can be safely removed,” said Tao Yu, a senior neurosurgeon.
Tumor grades played a decisive role in both functional prognosis and survival. Patients with high-grade gliomas were significantly more likely to develop permanent motor deficits, especially when they already had preoperative weakness. These patients also had shorter survival: median overall survival (OS) was 24 months for grade IV glioma, and median progression-free survival (PFS) was just 12 months. In contrast, patients with low-grade gliomas had substantially longer PFS and OS, particularly when tumors carried the IDH1 mutation.
Surgical outcomes also varied by tumor size and grade. Tumors larger than 24.5 ml and low-grade gliomas were more likely to undergo partial resection, reflecting the delicate balance between oncological control and functional preservation. Despite these limitations, many patients still achieved good long-term survival when treated with standard adjuvant therapy—radiotherapy, chemotherapy, or both—following surgery. “Our findings show that conservative, function-preserving surgery does not compromise long-term oncological outcomes when paired with appropriate adjuvant treatment,” noted Songlin Yu.
The authors emphasize that preoperative DTI tractography remains indispensable for assessing CST infiltration, anticipating surgical risk, and guiding intraoperative decision-making. However, they also caution that DTI alone has limitations, and integrating additional tools such as navigated transcranial magnetic stimulation may further improve accuracy. The study calls for multicenter validation and standardized imaging protocols to refine surgical strategies for motor-eloquent gliomas.
Overall, this work underscores the critical need for an individualized, function-sparing approach for patients with CST-infiltrating gliomas. While the risk of postoperative paralysis is high, thoughtful surgical planning combined with modern adjuvant therapies can still lead to meaningful long-term survival.
Reference
Wang, X., Zuo, Z., Yu, S. et al. Long-term clinical prognosis of patients with gliomas infiltrating corticospinal tract on DTI tractography. Chin Neurosurg Jl 11, 26 (2025). https://doi.org/10.1186/s41016-025-00412-8
About Chinese Neurosurgical Journal
Chinese Neurosurgical Journal is an open access, peer-reviewed journal publishing research in all areas of neurosurgery, including new trends in neurology and neuroscience, with a focus on clinical practice and techniques. It is the official journal of the Chinese Neurosurgical Society, which covers the publication costs, so authors do not pay article-processing charges. The journal aims to publish work from neurosurgeons and researchers worldwide. Articles are freely and permanently accessible online immediately after publication, promoting broad dissemination and exchange of neurosurgical knowledge globally. It supports advancements in neurosurgery through high-quality scientific contributions.
Website: https://cnjournal.biomedcentral.com/
About Professor Tao Yu from Beijing Tiantan Hospital, Capital Medical University
Professor Tao Yu, M.D., Ph.D., is a distinguished academic and clinician serving as a Professor of Neurosurgery at Beijing Tiantan Hospital and a senior researcher at the Beijing Neurosurgical Institute. He also holds an affiliation with the National Clinical Research Center for Neurological Diseases. Prof. Yu's core work centers on glioma surgery, neuroimaging, and corticospinal tract (CST) preservation. He integrates extensive clinical expertise with cutting-edge, imaging-based research to enhance surgical precision and optimize functional outcomes for patients. His contributions, detailed in peer-reviewed neurosurgical literature, solidify his reputation as a key figure in neuro-oncology.
Funding information
This research was funded by the Capital Health Development Scientific Research Project (No. 2022-2-1075 to Tao Yu).
Yi Lu
Chinese Neurosurgical Journal
1059978478 ext.
luyi617@sina.cn
Legal Disclaimer:
EIN Presswire provides this news content "as is" without warranty of any kind. We do not accept any responsibility or liability for the accuracy, content, images, videos, licenses, completeness, legality, or reliability of the information contained in this article. If you have any complaints or copyright issues related to this article, kindly contact the author above.